Tara Rynders
The views and opinions expressed by speakers and presenters in connection with Art Restart are their own, and not an endorsement by the Thomas S. Kenan Institute for the Arts and the UNC School of the Arts. This interview has been edited for length and clarity.
Tara Rynders is a dancer/choreographer and video artist based in Denver, CO. She is also a full-time registered nurse with over 15 years of experience. She combined her passions for dance and for compassionate care by creating The Clinic, an organization that through immersive artistic experiences combats compassion fatigue and professional burnout among nurses and fosters stronger connections between nurses, patients and communities.
Among the projects Tara has developed through The Clinic are “Resiliency Moments,” one-on-one virtual and intimate interactions between individual artists and healthcare workers in which art is made and grief and trauma begin to be healed.
Both the medical and artistic worlds have recognized Tara’s work. She received the highest level of nursing recognition in Colorado when in 2019 she was awarded the Nightingale Luminary Award, and she has received numerous arts grants, including a Blade of Grass Fellowship, to support her work melding the arts with science.
In this interview with Pier Carlo Talenti, Tara delves into how her experiences caring and being cared for in a hospital informed the creation of The Clinic and explains how more moments of back-and-forth empathy between artists and scientists could lead to substantial changes in the healthcare industry and beyond.
Choose a question below to begin exploring the interview:
- The work you currently do helps others, particularly healthcare workers, find their resiliency in gorgeous, inventive ways. Looking back to when you were maturing as an artist, do you have an idea of what would have contributed to your own resiliency and well-being?
- How did you decide to become an RN in the longer process of becoming an artist?
- Can you describe how you arrived at this fundamental belief that you have that the world of nursing could benefit from an injection of art and performance?
- How did you go about developing The Clinic?
- You said that dance is a way to keep yourself energized and alive. You have so much on your plate, so how do you keep your own wellbeing at the heart of what you do? How do you not burn out?
- As you know, we’re coming out of a year that was disastrous for so many artists, particularly performing artists. If you were to create a new workshop or version of “Resiliency Moments” that was targeted specifically to artists rather than healthcare workers, what would that look like?
- How did you find the time while working as a full-time nurse to do such a demanding project as “You and Me”?
- Has your own artistic expression at this point become synonymous with The Clinic and all its projects, or do you find you still need to find time and energy to work on your own personal art?
- The tagline for The Clinic is, “Reimagining the future of nursing through the arts and performance.” But I want to flip it. How could the future of the arts and performance be reimagined through nursing?
Pier Carlo Talenti: The work you currently do helps others, particularly healthcare workers, find their resiliency in gorgeous, inventive ways. You invited me to one of your “Resiliency Moments,” and it was a really, really remarkable experience. So thank you for that.
Looking back to when you were maturing as an artist, do you have an idea of what would have contributed to your own resiliency and well-being?
Tara Rynders: For me, dance and movement have always been my resiliency and space for me to feel and feel supported. I believe that we’re all resilient. We’re born resilient human beings; that’s just part of our makeup. And yet there are times when we fall out of that resilient zone, and that’s when we lean on other things such as dance, movement, family, support, community, whatever it may be. So for me specifically, it would be dance. I grew up dancing from a very young age, and that proved to be my safe space where I can feel my feelings.
Pier Carlo: And how did you decide to become an RN in the longer process of becoming an artist?
Tara: Growing up, I wasn’t necessarily encouraged or didn’t even know it was an option to be an artist and a dancer as my career. I knew growing up that I had friends who did it, but in my mind it wasn’t ever really laid out as an option. I always had this idea that I’m a dancer, I know I’m a dancer, I know I’m an artist and I’ll always be that, but at the same time my mother taught me at a very young age that I would have to really be able to make my own money and be able to stand on my own financially. I didn’t think that was possible through the arts, and so I always was thinking, “What else could I do?”
One of my favorite things is being present with someone in their most difficult times, just because it’s a very real, sacred experience to be alongside someone in that journey, and so I felt nursing really encapsulated that whole experience for me.
I really loved caring for people when people were sick and nurturing them. One of my favorite things is being present with someone in their most difficult times, just because it’s a very real, sacred experience to be alongside someone in that journey, and so I felt nursing really encapsulated that whole experience for me.
Pier Carlo: So as you went to nursing school, it didn’t feel like you were turning your back on your artistry at all?
Tara: No, never. I danced the whole time. I’ve always been one to incorporate and collaborate and bring worlds together that maybe at first don’t seem like they fit, but for me it was always really important to have this sense of wholeness and not feeling separated into different things. So I danced and created and choreographed all throughout nursing school.
Pier Carlo: And what was your mission as a dancer, choreographer? What was your mission as an artist?
Tara: I really didn’t have a mission. I think it was to stay alive. [She laughs.] I think that it was a survival for me. Like I said, it was my resiliency. Through all the things in life that gets thrown at us, there really wasn’t an option to not be an artist or a dancer for me. It always felt like that was who I was in my core.
Pier Carlo: Can you describe how you arrived at this fundamental belief that you have that the world of nursing could benefit from an injection of art and performance?
Tara: I think because art and performance really makes sense to me. It’s where I really feel things deeply.
I was a patient for the first time when I had an ectopic pregnancy that had burst and I was rushed to emergency surgery. But before that I had passed out. I just remember that whole experience being a patient of really watching everything and being on the other end of care, watching the way nurses and the physicians treated me and my body and when my physician sat down to talk to me and came face to face, really appreciating that. I was experiencing this ectopic pregnancy but also watching it from afar and taking it in from a new view that I had never had before. I had, but not to this extent where it was so scary.
When I passed out, the nurse called a code yellow, which is the code you call before a code blue when you stop breathing. It’s a precursor, like, “Help, we’re going down the wrong path here.” Everybody runs into my room and I’m passed out, and I just remember being so scared.
Pier Carlo: You were at work when this happened?
Tara: I wasn’t. I drove myself to the hospital. I found out that morning I was pregnant, and that evening I had just so much pain. I had six-month-old twins at the time, and so that whole situation in itself was crazy. We couldn’t wake up our babies because they were sleeping, so I drove to the hospital, and it all started to really unravel really quickly. In the midst of all of it — again, like I said, watching it from this third-eye view almost and then experiencing it — I remember being passed out, everybody running in, them hanging blood and putting my head down and my feet up so that my essential organs would get what they needed. And then the nurse, she grabbed my hand and she said, “I’m here, and you’re going to be OK.”
I really believe in moments ... that moments can really shift things, and that shifted it for me, to feel seen by my nurse in that way even though I was completely passed out.
At first I didn’t really want to hold her hand. I was just really trying to be strong. I was like, “I don’t need that.” Then I relaxed into her hand, and I remember just thanking her. Really in a deep way in my mind I remember saying, “Thank you for remembering me because I’m so scared and I couldn’t speak myself.” That moment! I really believe in moments — just like we created “Resiliency Moments” — that moments can really shift things, and that shifted it for me, to feel seen by my nurse in that way even though I was completely passed out.
That’s when I knew. I didn’t realize as a nurse how impactful I could be in so many situations because you forget, and so I wanted to just help nurses remember how important and valuable they are to our patients.
Pier Carlo: How did you go about developing The Clinic, which is now a multi-pronged program? How did you work that out? And how did you get healthcare workers to buy into it?
Tara: It was in 2016 that I had this experience, and then I knew I needed to raise awareness around it first. I first did this experience with nurse leaders. I asked my chief nursing officer, “Can I just have some time on the next agenda?” and I walked them through some art-based experiences to help them feel what it’s like to be a patient because that was so impactful for me. And then also some hands-on touching things with each other and to build community among the leaders. That was really fun.
But then I was like, “They need more. We need to understand more.” So that’s when I worked with some artists, Lia Bonfilio, who is an immersive theater performer out of New York city, and Jadd Tank, who was living in New York City at the time, who’s also an amazing performing artist.
The three of us created “First Do No Harm” alongside Edith Weiss, who co-wrote the script with me. We created an immersive theater performance that took place in the hospital, and we opened it up to the public. They came in and they followed this story, this narrative told from the perspective of the patient’s partner and the nurses, so really perspectives that you don’t hear from very often in the hospital, and we walked them through what it looked like for nurses, what their shift was like. They did these monologues on compassion fatigue and burnout. At the time, gosh, nobody was talking about this. There was a lot of stigma around our burnout and our wellness. That was the first step, really raising awareness.
The nurses who came to see that, they were like, “Wow!” They told me, “I felt really seen. Thank you for sharing my story. I never had words before to really express what I was going through, and you gave me those words.” So that felt really successful for them to acknowledge that.
Pier Carlo: So it was always assumed that nurses never had compassionate fatigue, it was just something that was never talked about?
Tara: Right. Yeah.
Pier Carlo: You said that dance is a way to keep yourself energized and alive. You have so much on your plate, so how do you keep your own wellbeing at the heart of what you do? How do you not burn out?
Tara: I think self-compassion, because I mess up a lot. [She laughs.]
Pier Carlo: How so? How do you mess up?
Tara: I feel like there are so many balls that I’m carrying, and I drop them quite often. It’s about being in relationship with myself and others so that when I do drop those balls, I go and I say, “I’m sorry I dropped that ball.” Then it’s having that conversation, “Are there too many balls right now? What can I get rid of or set aside for a moment? Who can I bring in to hold this for me, because I can’t?”
I’ve just recently experienced this with “Resiliency Moments” and was able to bring in a program manager. I was getting the hospitals to sign on and getting the contracts for that and at the same time implementing and hiring artists and bringing them in, and then things were falling through the cracks. So I had to go back to everyone and say, “I’m sorry, I’m not able to do this.” And we had a really great debrief with the whole team where people were like, “Well, I would like to do this. I can do this.” It also breaks down the hierarchy of me being the only one. So now we’re looking at it more of as a collaborative experience process where the artists are also holding these spaces that I once did.
Then the relationship with myself of always checking in: “Is this too much? What can I offer over to someone who may be wanting this or needing this at this time in their life too when I don’t need to hold onto it?”
Pier Carlo: Was that difficult? Was it difficult to let go of control of your baby?
Tara: Oh yeah [laughing]. I think you’ll hear this a lot with nurses. I think it’s a really interesting point that a lot of our burnout and fatigue is rooted in our need to control because for most of us as nurses, these are our patients, we’re in charge of them, we are the ones responsible for them. So sometimes that means we’re not going to go on a lunch break because we don’t trust that the other nurse is going to watch our patients for us in the way that we feel they need to be watched. We’ve created a lot of this culture. I’m not saying we’ve completely done this, because it’s very much in the system, but we’ve also bought into this culture of, “I can be the only one to do this,” and that way of thinking, which leads to burnout.
Pier Carlo: As you know, we’re coming out of a year that was disastrous for so many artists, particularly performing artists. If you were to create a new workshop or version of “Resiliency Moments” that was targeted specifically to artists rather than healthcare workers, what would that look like? Would it be at all different?
Tara: That’s a really good question. I think there’s been something really beautiful about Resiliency Moments actually caring for artists at the same time. It’s the artists leading the moment for healthcare workers. But from the feedback, artists are just garnering so much from being the one to create the space for others, and because it is interactive there’s a sense of healing that goes back and forth. It’s that type of structure that I also think is missing in the hospital, where we come in and we take care of our patients and yet the relationship can be missing where it’s very one-sided. So it’s creating these spaces for real relationships to occur.
Artists are also empaths, so they’re empathizing with healthcare workers and they’re receiving at the same time. I think 'Resiliency Moments' really was created for everyone.
When I’m caring for a patient, if their story moved me, I want to sit and I want to cry with them. And I think that’s OK, not to the extent where they’re taking care of me but that I’m showing that empathy. Artists are also empaths, so they’re empathizing with healthcare workers and they’re receiving at the same time. I think “Resiliency Moments” really was created for everyone.
It comes from a performance called “You and Me” that I did in-person in 2007 and for many, many years and toured nationally and internationally to different locations. It’s about intimacy and having these one-on-one in-person experiences. And it was for everyone, and everyone benefited and really enjoyed it.
Pier Carlo: Can you describe “You and Me”?
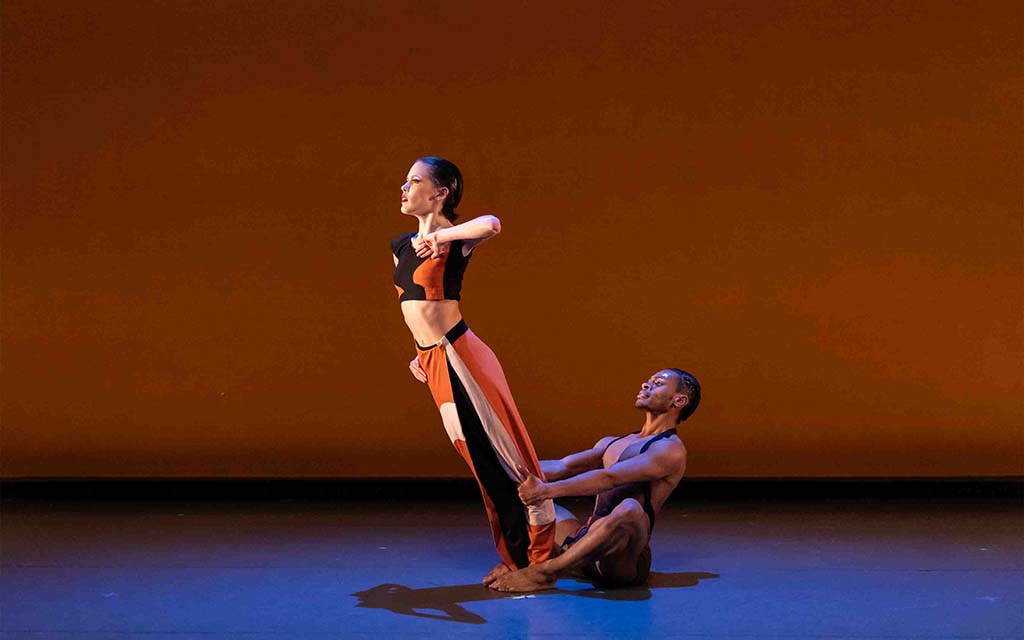
Tara: I can. It’s a three-hour durational performance that opens with a big opening dance. That usually was a duet between myself and one other person. One of the performances, we started at the top of this mountain and so you could just see us really, really tiny. And then we ran down the face of the mountain, stopped halfway and did a dance and then slowly made our way. And then we swam in this creek to finally meet the audience. It was playing with perspective and intimacy and how close can we get.
There’s an opening performance. We know everyone who’s coming ahead of time, so when everyone arrives we make a big circle and we have appointment cards with maps. When they say their name, we run and we give them a card with their name on it with an appointment and a map. And then they go have these one-on-ones; they follow the map to where their appointments are. It was really based in many ways on the emergency room as I was working as an ER nurse, going into these almost little clinic spaces but they were curated and created by artists. Similar to “Resiliency Moments,” we had these short interactions with each other that were really profound in many ways because I think they were only five minutes long when we did them in person, so you had to really just jump right in. Then we had a sit-down family-style dinner at one long table, and everyone ate together. Then there was a dance on the table afterwards.
It really was in my mind a little bit of what connection and intimacy and maybe even heaven would feel like here on earth with people we don’t necessarily know coming together to care for one another. It came out of when my sister was really sick. She was in a coma for many months, and I moved into her rehabilitation room and bathed her and was her voice because she couldn’t speak. It came out of this desire to bring back intimacy into our connections with one another.
Pier Carlo: How did you find the time while working as a full-time nurse to do such a demanding project as “You and Me”?
Tara: During that time, I got my master’s in dance, and I worked per diem as a nurse.
Pier Carlo: You got your master’s in dance after you became an RN?
Tara: Correct, yep. I worked full-time the first year and it was way too much, so I went to PRN [“pro re nata,” when needed], which was wonderful, so I was able to focus more. It was my last semester of school that my sister got sick, and so I took that semester off and graduated later and came back. “You and Me” was my thesis performance because it was after that experience. Doing a concert dance, stage dance, just didn’t seem possible for me. I really wanted something more intimate based on what I had just experienced. After I did “You and Me” as my thesis, we decided to tour it, and I continued to work per diem during that time.
Pier Carlo: Has your own artistic expression at this point become synonymous with The Clinic and all its projects, or do you find you still need to find time and energy to work on your own personal art? Are they the same thing?
Tara: They used to be, but as The Clinic is growing, my role has shifted. It just depends on the season. I recently was able to film a bunch of short dances for camera. That was based in resiliency for nurses, but it did feel like a lot of my own artistry in it. It was really beautiful to see that blend happen again, but it had been a while mostly because of COVID. I had a one-woman show planned for the spring called “A Nurse’s Calling,” and now that’s been pushed back to the fall. I try to hold those worlds together and make them blend as much as possible just for my own heart to be creating.
Pier Carlo: Can you describe “A Nurse’s Calling”?
Tara: Sure. “A Nurse’s Calling” is going to be based in an ambulance. It’ll be a traveling performance that’ll go in different communities. Really it’s sharing stories around burnout, around COVID, and also a call to action for our own accountability as healthcare providers — well, to everyone but specifically healthcare providers and nurses — checking our biases in racism and knowing the role we play in health-equity issues. It’s been something that I’ve just been researching a lot and personally reflecting upon. In what ways do I uphold racism at the bedside with my patients based on personal biases or whatever it may be? And how do I participate in it with physicians who may say something?
For example, if I say, “Oh, I think this patient who happens to be Black needs pain medicine,” and the physician may say, “Oh, well that patient is always here” — whatever the conversation is — but it’s evident that he’s going to be treating this patient differently based on bias, experience, whatever it may be, racism, I don’t know. But I have a choice in that moment to say, “OK,” and walk away and not give that patient pain medicine, which the research shows many of our Black patients are not receiving as much pain medicine as white patients. I have a choice to say, “OK,” and walk away, or I can say, “I really see this patient in pain. Can you please order him something?” And push back. There’s a lot there I think we’re still unraveling.
Pier Carlo: How does the piece address that in an ambulance?
It’s really just telling the truth, telling the truth about what I’ve seen and what I’ve done myself and experienced and opening that up for people to tell their truth as well.
Tara: It’s telling that story. It’s telling my stories, my experiences of seeing Black patients die in the emergency room and people saying, “Oh,” and that’s it, versus, “Well, what happened here? Was there something else that we could have done?” And then watching that experience happen with a white patient, a very similar experience, and having a very different response to it. It’s really just telling the truth, telling the truth about what I’ve seen and what I’ve done myself and experienced and opening that up for people to tell their truth as well.
Pier Carlo: It’s so interesting that you say, “Telling the truth.” It feels like right now in this country people are holding onto very different, alternate truths, I think especially around issues of race. How can your work bring people together to one truth?
Tara: Yeah, that’s a really good question, and I don’t know if there really is one truth.
Pier Carlo: Well, your work is based on research and fact, so that is one kind of truth.
Tara: That’s true, right. And I think it’s bringing that research to life through retelling, laying the groundwork: “This is the research, this is what is happening, and it’s not fake. It’s real, and this is how I experienced it in real time.” Then giving resources: “And this is what we can do to do things differently in the future.”
A lot of the work that The Clinic is doing in the future is also including anti-racism training for nurses and grief recovery for nurses, so they have this space to self-reflect as well on the ways they uphold racism.
Pier Carlo: The tagline for The Clinic is, “Reimagining the future of nursing through the arts and performance.” But I want to flip it. How could the future of the arts and performance be reimagined through nursing?
Tara: Yeah, I love that question. I think it’s a little bit what we’re doing with “Resiliency Moments” on tapping into this empathy that you’ve talked about with artists and the connections that they can offer in the relationship and these intimate spaces that they can create.
There’s been a really interesting training that we do with our artists that is based in nursing theory. They’re learning all about “See Me as a Person” and relationship-based care, what nurses learn as they create these safe spaces between themselves and their patients. We put our artists through those trainings where they come out with these tools of how to really, truly see another person, connect with them and use their art to be the driver for that. And it’s really powerful.
Pier Carlo: I love the idea that you’re showing artists that they have it in themselves to be healers.
Tara: Yeah, exactly. And I think in many ways they come out of that training saying, “Oh, this is what we do.” It’s not like I’m bringing anything fancy to them. “This is already in you. It’s just reminding you that this is so important and you have this ability.”
August 09, 2021